Female & Male Genitalia - ppt video online download
4.7 (128) · $ 19.50 · In stock
Female Health History Menstrual History Obstetric History Age at menarche, frequency & duration of menstrual cycle, character or flow (amount and presence of clots), presence of dysmenorrhea (painful menstruation), dates of last two menstrual periods and premenstrual symptoms. Bleeding outside of period or during menopause Ie. Endometriosis, endometrial cancer Obstetric History Number of pregnancies, miscarriages or abortions, or complications
Female & Male Genitalia
Age at menarche, frequency & duration of menstrual cycle, character or flow (amount and presence of clots), presence of dysmenorrhea (painful menstruation), dates of last two menstrual periods and premenstrual symptoms. Bleeding outside of period or during menopause. Ie. Endometriosis, endometrial cancer. Obstetric History. Number of pregnancies, miscarriages or abortions, or complications.
Prevent against cervical cancer & genital warts. Symptoms of infection/STIs. Vaginal discharge, pelvic pain, swollen perianal tissues or genital lesions. Symptoms of genitourinary problems. Burning during urination (dysuria), frequency, urgency, nocturia, hematuria, incontinence, stress incontenence. Symptoms of Perimenopause. Hot flash, drenching sweats, mood swings, vaginal dryness, itching, numbness and tingling, headache, or palpitations.
>40 y/o, obese, history of ovarian dysfunction, breast or endometrial cancer, irradiation of pelvic organs, endometriosis, infertility or nulliparity, use of estrogen only hormone replacement. family history of ovarian, breast, or endometrial cancer. Risk factors for endometrial cancer. Postmenopausal, obese, infertile, early menarche, late menopause, HTN, DM, gallbladder disease, PCOS, estrogen-related exposure (HRT or tamoxifen use) Family history of endometrial, breast, or colon cancer.
Sexual history and current/past contraceptive practices. Oral contraceptives- Ask about tobacco use, history of blood clots due to increased risk for blood clots. Previous illness or surgery involving reproductive organs, including STIs.
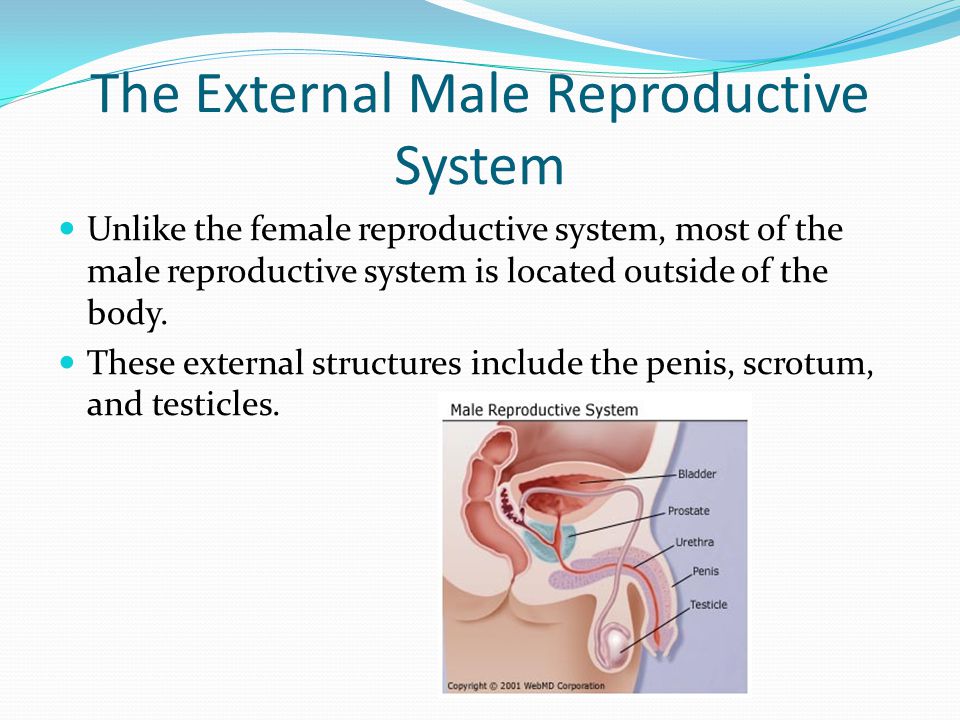
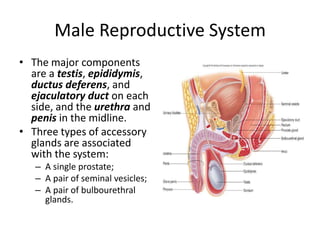
Frequency, nocturia, urgency, decreased urinary output, difficulty starting stream, hematuria. Penile pain or swelling, genital lesions or urethral discharge. Heaviness or painless enlargement of testis or irregular lumps. Performance of self testicular exam Presence of inguinal hernia. Difficulty achieving erection or ejaculation.
Offer a chaperone. Keep patient draped for privacy. Avoid unexpected or sudden movements. Watch patient’s face to monitor comfort. Wear gloves.
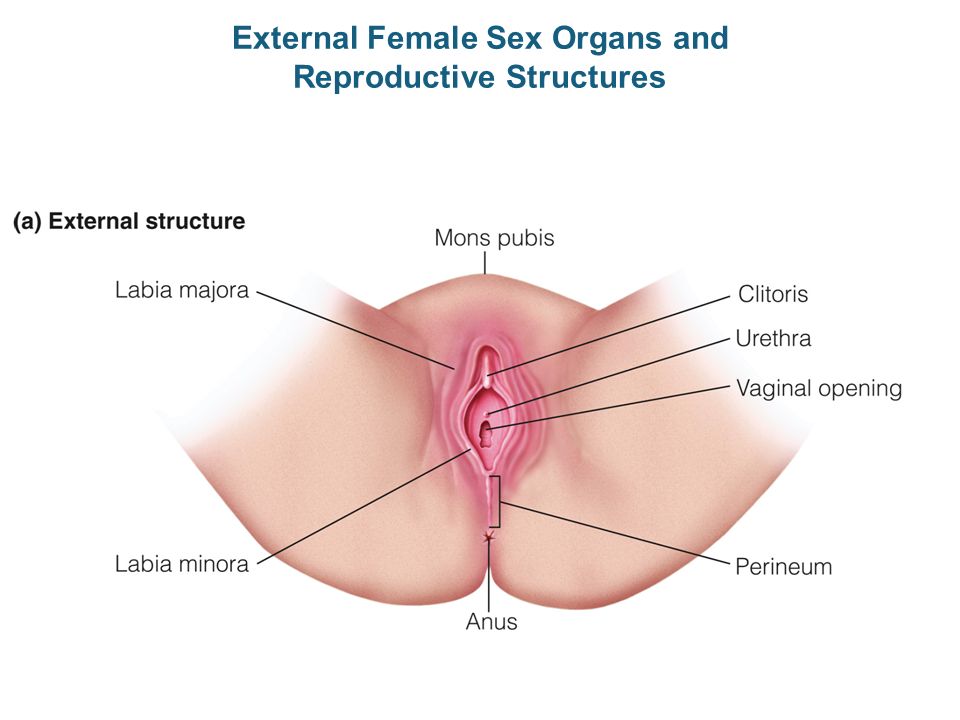
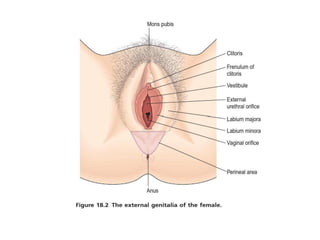
No suspicious pigmented lesions noted. Hair distribution. Inverted triangle. No nits or lice. Tanner staging for adolescence. Note: The nurse will often examine external genitalia while performing routine hygiene measures or preparing to insert a urinary catheter.
Symmetrical, no excoriation, nodules, rash, lesions or edema. Perineum. Smooth. Well healed episiotomy scar.
Labia minora. Dark pink and moist. Urethral opening. Slitlike and midline. Vaginal opening. No discharge or foul odor. No excoriation, nodules, rash, lesions, or edema.
BV- thin, creamy gray-white; foul smelling. Trichomoniasis- frothy yellow-green; foul smelling. Chlamydia- White mucopurulent. Gonorrhea- yellowish.
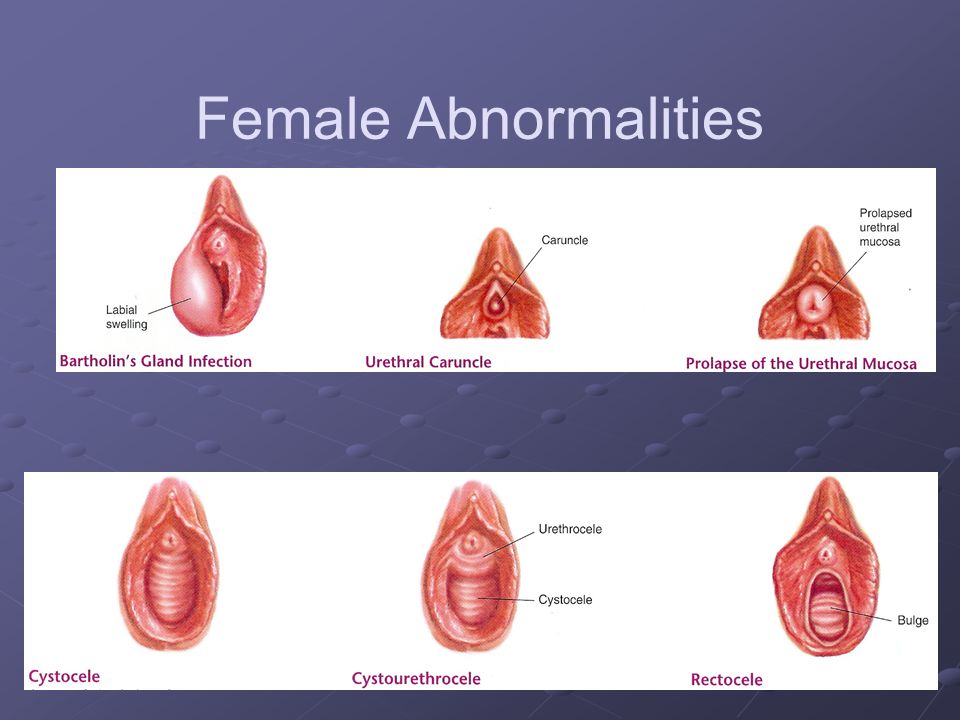
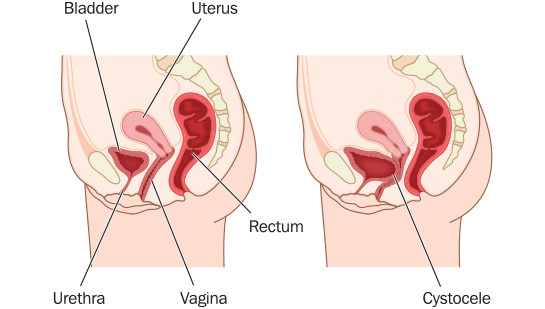
Female Abnormalities Rectocele Cystocele Uterine prolapse
be on menses. Patient should avoid intercourse, douching, vaginal suppositories and tampons 24 hours prior to exam. Have patient empty bladder before examination. Patient lies supine, with head and shoulders elevated. Have patient place heels in stir-ups, slide all the way down examination table until buttocks extend slightly beyond the edge. Thighs should be flexed, abducted and externally rotated at the hips. Have light source available and supplies accessible.
Obtain cervical smears and cultures. Pap Smears for cervical cancer. Inspect vaginal wall and cervix. Palpate cervix, uterus & ovaries.
Winkled, hairless, without lesions or inflammation. Dorsal vein may be apparent.
May need to retract foreskin. Phimosis- unable to retract foreskin. Paraphimosis- Unable to return foreskin to original position. Smegma- Cheesy substance under foreskin.
Urethral meatus. Positioned centrally. Hypospastic- ventral location. Epispadias- dorsal location. Compress glans anteroposteriorly between thumb and forefinger to assess for dc. Meatus pink, smooth, without discharge. Profuse yellow = gonococcal. Scanty white = possible Chlamydia.
Assess for nodules, induration, or tenderness. Smooth, semifirm, and nontender. If man gets erection during the exam, explain that it is a normal response and finish the exam.
Mild asymmetry normal. Left often lower than right. Assess for edema and lesions.
Testes- freely movable, oval, firm, rubbery, smooth and equal bilaterally.
Spermatic cord- smooth and nontender.
Palpate femoral areas for bulge. No femoral hernia noted.
Palpate inferior to inguinal ligament and along upper inner thigh. Normal to palpate isolated node on occasion. Nonpalpable or small (<1cm), soft, discrete, and movable.
If found early, excellent prognosis. The best time to examine testicles is during or after a shower or bath. The warm water allows the scrotum to relax and the testicles to drop down. The left testicle normally hangs a bit lower than the right. It is common for one testicle to be larger than the other one. Young men should examine themselves once a month. More frequent exams actually may result in missing a slowly changing lump.
Gently roll each testicle between the thumb and fingers. Testicles should feel firm and smooth, about the consistency of a hard-boiled egg without the shell. The epididymis is a ropelike structure attached to the back of the testis. This structure is not an abnormal lump. Feel for firm masses, lumps, or nodules in the testicle. In cancer, these lumps often are painless. Become familiar with normal size, shape, and weight of each testicle and epididymis. This will help you recognize a change from one self-examination to another, if a change should occur.
External Female Sex Organs and Reproductive Structures - ppt video

Male reproductive organ - PowerPoint Template

Male reproductive system

Biology: Human Reproduction
The Male Reproductive System - ppt video online download
Development of the male& female genital system.pptx

Female reproductive system
Reproductive system
Genitalia. - ppt video online download

assessment of the female genitalia
Male and Female Reproductive Systems - ppt video online download

Female & Male Genitalia - ppt video online download
Human reproduction 3d, human reproductive system 3d
Male reproductive system






:max_bytes(150000):strip_icc()/GettyImages-155358151-b8d59990d3154105a946aa712745f2c6.jpg)